In this retrospective, multicenter study, the accuracy of Transpara, used for breast cancer detection, was investigated in a Danish mammography screening population. The AI system was evaluated in a simulated AI-standalone scenario and a simulated AI-integrated scenario replacing first reader. In both scenarios, two AI-score cut-off points were applied by matching at mean first reader sensitivity and specificity. The authors suggest that an AI system with an appropriate threshold could be feasible as a replacement of the first reader in double reading with arbitration.
Read full study.
*As an interesting note: the same dataset was used for the evaluation of Lunit. That paper came out just two months earlier, find it in our November newsletter.
Abstract
Background
Artificial intelligence (AI) systems are proposed as a replacement of the first reader in double reading within mammography screening. We aimed to assess cancer detection accuracy of an AI system in a Danish screening population.
Methods
We retrieved a consecutive screening cohort from the Region of Southern Denmark including all participating women between Aug 4, 2014, and August 15, 2018. Screening mammograms were processed by a commercial AI system and detection accuracy was evaluated in two scenarios, Standalone AI and AI-integrated screening replacing first reader, with first reader and double reading with arbitration (combined reading) as comparators, respectively. Two AI-score cut-off points were applied by matching at mean first reader sensitivity (AIsens) and specificity (AIspec). Reference standard was histopathology-proven breast cancer or cancer-free follow-up within 24 months. Coprimary endpoints were sensitivity and specificity, and secondary endpoints were positive predictive value (PPV), negative predictive value (NPV), recall rate, and arbitration rate. Accuracy estimates were calculated using McNemar’s test or exact binomial test.
Results
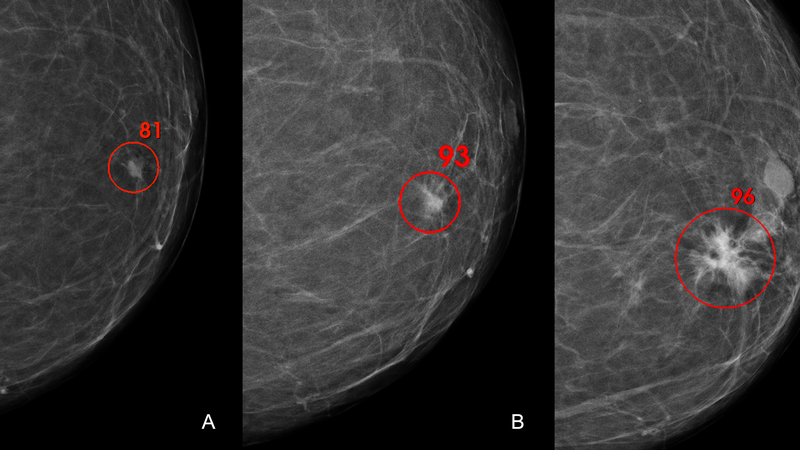
Out of 272,008 screening mammograms from 158,732 women, 257,671 (94.7%) with adequate image data were included in the final analyses. Sensitivity and specificity were 63.7% (95% CI 61.6%-65.8%) and 97.8% (97.7-97.8%) for first reader, and 73.9% (72.0-75.8%) and 97.9% (97.9-98.0%) for combined reading, respectively. Standalone AIsens showed a lower specificity (-1.3%) and PPV (-6.1%), and a higher recall rate (+ 1.3%) compared to first reader (p < 0.0001 for all), while Standalone AIspec had a lower sensitivity (-5.1%; p < 0.0001), PPV (-1.3%; p = 0.01) and NPV (-0.04%; p = 0.0002). Compared to combined reading, Integrated AIsens achieved higher sensitivity (+ 2.3%; p = 0.0004), but lower specificity (-0.6%) and PPV (-3.9%) as well as higher recall rate (+ 0.6%) and arbitration rate (+ 2.2%; p < 0.0001 for all). Integrated AIspec showed no significant difference in any outcome measures apart from a slightly higher arbitration rate (p < 0.0001). Subgroup analyses showed higher detection of interval cancers by Standalone AI and Integrated AI at both thresholds (p < 0.0001 for all) with a varying composition of detected cancers across multiple subgroups of tumour characteristics.
Conclusions
Replacing first reader in double reading with an AI could be feasible but choosing an appropriate AI threshold is crucial to maintaining cancer detection accuracy and workload.
